
cataracts
Introduction
Good vision depends on many factors. One factor is the transparency of the
eye structures in the line of sight. Any disturbance in the clarity may
impair best visual acuity or cause problems with glare or cause other
visual distortions and distractions. Cataracts cause a clouding with
distortions and lack of clarity in the lens of the eye. This is a very
common condition with over one million surgical procedures for cataracts
performed each year in the United States.
Anatomy of the Eye
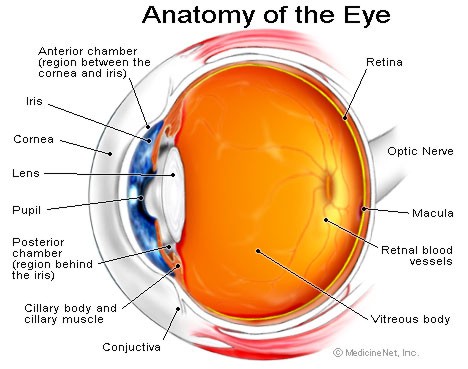
The anatomy of the eye is similar
in many ways to a camera. Moving from the outer portion of the eye to
inner, light passes through several structures before falling on the
retina (equivalent to a camera's film), where the brain may process the
light as a visual image. First, light passes through the cornea, the clear
portion of the outer eye that contact lenses are placed on. This area is
sensitive to touch and is similar to a filter placed over a camera's lens.
It usually remains clear unless there is an infection with scarring,
trauma or vision correction surgery with complications. Underneath the
cornea is the anterior chamber filled with a clear fluid called aqueous
humor. This aqueous humor is constantly flowing through the anterior
chamber except in conditions that may block the outflow. This will cause a
rise in the pressure in the anterior chamber and may lead to glaucoma. The
lens lies just under the coloured iris and forms the back of the anterior
chamber and the front of the posterior chamber. The lens is visible
through the opening in the iris called the pupil. Behind the lens is the
posterior chamber filled with a clear jelly-like protein termed the
vitreous humor. The inner lining of the back portion of the eye is the
retina.
The lens is a convex disk that is held in place by muscles. The outer
lining of the lens is called the capsule. The lens changes shape by
contracting and relaxing the ciliary muscles to change the focal distance
of the eye by making the lens thicker or thinner. The younger lens can
change shapes rather dramatically allowing reading at very close distances
when the lens is thicker. Cataracts occur in the lens of the eye.
Aging and Presbyopia
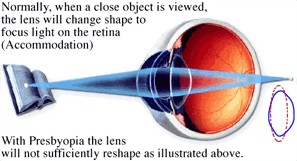
Aging causes several effects in
the eye. One is a stiffening of the lens and a progressive loss of the
lens' ability to change shapes. The individual finds that reading must be
done at greater distances initially and then with the aid of reading
glasses. This stiffening of the lens with age is termed presbyopia.
Presbyopia is a universal phenomenon.
Cataract Formation
Cataract formation is also a consequence of aging, although it is by no
means a universal finding like presbyopia. There are other causes of
cataracts. These may include inherited conditions, trauma or exposure to
microwave or UV radiation. Pilots are at risk for microwave
radiation-induced lens damage if they were to repeatedly stand in front of
an operating weather radar on the ground. Cataracts are irregular
collections of protein densities within the lens. These imperfections
distort light flow through the lens. This is analogous to imperfections in
a diamond or cracks in a clear ice cube. The lens begins to cloud as a
cataract grows. Cataracts tend to be progressive in size and density,
obscuring vision as they grow. They consolidate in a process called
maturation.
Effects on Vision
If the cataract is off the central visual axis, it may not be noticed in
daylight when the pupil is small and light passes through the lens without
striking the cataract. At night, the pupil opens wider to get more light
to the eye. The cataract may bend light entering the periphery of the
lens. A person may perceive this as glare or halos around lights at night.
If the cataract is on the central visual axis (near the center of the
lens), best visual acuity will gradually deteriorate. Glasses do not help
overcome the interfering effects of the cataract on light passing through
the central portion of the lens.
FAA Vision Standards
A pilot or controller may perform aviation duties with a cataract as long
as he/she meets the visual standards for the class of medical certificate
applied. The distant standard is 20/20 corrected for First and Second
class certification and 20/40 for Third class certificates. Once the
standards can not be met, the pilot is grounded. Surgical options with
replacement of the lens with an artificial implant offer the best
opportunity to meet standards. Intraocular lenses (IOLs) are made of
synthetic plastics such as PMMA. Use of IOLs is allowed for all classes of
certification. A pilot may have IOLs in both eyes and still be waived for
First Class certification.
An ATCS may be granted permission by the Regional Flight Surgeon to
continue to control if a cataract degrades vision to 20/25 in one eye.
Typically however, unilateral vision loss or field defects are not
acceptable for air traffic control operations in a tower. They may be
waived for pilots, however.
Surgical Correction and Intraocular Lenses
The surgery to remove a cataract and implant the lens is generally well
tolerated. The cataract must be mature enough to allow removal. There are
several techniques to use. Most involve making a small incision on the
edge of the cornea to access the lens. The contents of the lens within its
capsule is emulsified and removed with suction. An artificial lens (IOL)
is placed in the capsule and anchored in place with one or two sutures.
The cornea is then sutured and heals quickly. The corneal sutures are
removed in several days. Most pilots note a dramatic improvement in their
distant vision immediately. Because the artificial lens does not change
shape, near vision for reading usually requires glasses.
The FAA does not approve multifocal intraocular lenses. Insertion of this
type of lens may result in permanent grounding. For pilots who have
bilateral IOLs inserted with one focusing at distant and one focusing at
near, pilots will be denied medical certification for a minimum of six
months. If they are able to adapt to the vision adequately, they may be
granted a Statement of Demonstrated Ability (SODA) for functional
monocularity. The FAA discourages this approach.
A new self-accommodating IOL (can focus both at distant and near) was
approved by the FDA in November 2003. The Crystalens uses the muscles of
the eye to move the lens and adjust the focal distance. This new lens may
negate the need for reading glasses. The FAA may consider authorizing the
lens after November 2004.
FAA Reporting Requirements
Once a pilot meets FAA vision standards, they may return to flying on
their current medical. We suggest discussing this with the Aviation
Medical Examiner to maker sure they will grant a medical when it comes due
without the need to defer. Controllers are required to report to the
Regional Flight Surgeon before returning to duty. The pilot or controller
should provide the operative report, a statement about what IOL was used
and an FAA Form 8500-7, Report of Eye Evaluation completed by the
ophthalmologist at the final visit following surgery.
The reports may be mailed by the pilot to the FAA at:
Federal Aviation Administration
Aeromedical Certification Division
CAMI Bldg./ AAM-300
P.O. Box 26080
Oklahoma City, OK 73126-9922
However, incomplete packages or inadvertent statements by treating
specialists sometime trigger undue scrutiny by the FAA. Our VFS physicians
may also assist in expediting FAA reporting and clearance, and are trained
to recognize and help your physicians properly address any aeromedically
significant issues before submission.
|
