
gallstones
and gallbladder disease

Introduction
Gallstones (cholelithiasis) and inflammation of the gallbladder (cholecystitis)
affect over one million people in the US each year and 16-20 million
Americans have gallstones. 500,000 surgeries are performed every year to
remove gallbladders and stones. For the pilot and controller, this
condition presents minor medical certification issues. Reporting to the
FAA is usually rather straight forward.
Anatomy of the Gallbladder
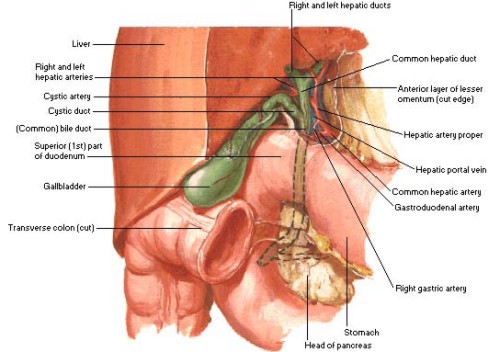
The
gallbladder is a large thumb sized sac that stores bile produced in the
liver. A system of connecting tubes known as ducts direct transfer of the
bile between the liver, the gall bladder and the small intestine, where
the bile aids in the digestion of fats and cholesterol. This system is
known as the bilary system. Think of the three ducts as forming a "Y".
Bile produced in the liver drains down one upper arm of the Y through the
hepatic duct. It moves up the upper arm of the Y, called the cystic duct,
to be stored in the gall bladder until it is needed for digestion. The
gallbladder then squeezes bile through the cystic duct into the common
bile duct which makes the lower leg of the Y. A muscle around the base of
the common bile duct relaxes to allow bile to flow into the intestine for
aid in digestion.
Stone Formation and Risk Factors
As long as there is unobstructed flow of bile through all three legs of
the Y, problems rarely occur. If one or more of the legs are blocked,
pressure can build as bile is continuously produced but not released. This
can cause pain and inflammation. Bile may sometimes form into stones from
the size of sand grains to nearly golf ball sized. The stones are composed
primarily of cholesterol and tend to occur when cholesterol concentrations
in the gall bladder increase compared to bile acid concentrations. These
stones may get stuck in the cystic duct and block the outflow. Less
commonly, they may get stuck in common bile duct and block flow of bile
from both the liver and the gallbladder. This is very serious and a person
quickly becomes ill and jaundiced. Ironically, the smaller granular stones
tend to clog the ducts more frequently. The larger stones tend to sit in
the gall bladder, rather than move down the ducts, because they are so
large. They may not cause any symptoms at all.
Risk factors for gall stone formation include obesity, rapid weight loss
by fasting, high fat diets, female hormones, increasing age, pregnancy,
sludging in the gall bladder and some medications.
Gallbladder Disease Symptoms
Gallstones frequently manifest themselves by a cramping pain below the
right rib cage after eating. Fatty meals may be particularly provocative.
In more serious cases, the pain can be incapacitating and confused with
ulcers, heart disease, kidney stones or pancreatitis. If associated with
fever, the condition requires immediate medical attention to treat the
cholecystitis. Sudden pain in the right upper quadrant of the abdomen that
may radiate to the right shoulder blade is termed "bilary colic." It may
persist for 1-4 hours and is followed by a dull upper abdominal pain for
about a day. The symptoms may be precipitated by a high fat meal (the FBO
"special") and relieved by limiting intake to non-fat liquids.
Initial treatment may include restricting oral intake to clear liquids or
nothing at all. Intravenous fluids, restricting oral intake, and
occasionally using a nasogastric tube to drain the stomach contents, will
allow the gallbladder to calm down. Fever and an elevated white blood cell
counts dictate the use of antibiotics. Surgeons are very reluctant to
operate while someone has a fever as the complication rate rises
dramatically. Many mild cases will not recur for extended periods,
particularly if one is cautious with their diet. Forgetting about the diet
may provide an uncomfortable reminder of the condition. Frequently, mild
symptoms may be treated with dietary restriction and watchful waiting.
This watchful waiting is an acceptable management technique. Many men will
have asymptomatic, or "silent" gallstones and up to 80% may never have any
symptoms nor require surgery.
Diagnosis of Gallstones
The definitive test to verify the presence of gallstones is the
gallbladder ultrasound, which gives a two dimensional picture using
Doppler imaging techniques to show the location and size of the stones.
Blood tests may lead to the suspicion of gall bladder disease with
elevated liver function tests and bilirubin. Occasionally, the diagnosis
is made by visualizing the stones during an x-ray or CT scan. Only 10-15%
of stones contain enough calcium to be visible by x-ray. To evaluate
inflammation and function of the gall bladder, scans using radioisotopes
injected in the blood and visualized with a nuclear imaging camera are
sometimes used. They are most useful in acute inflammation of the gall
bladder. Finally, an Oral Cholecystogram (OCG), which was the primary
diagnostic tool before ultrasound, is useful in assessing the function of
the gall bladder and ducts in those people who are not surgical
candidates.
Treatment
For people with recurrent gall bladder symptoms, both medical and surgical
techniques are available to treat the condition. Most commonly, surgery is
used to remove the gallbladder and its stones. The bile no longer is
stored in the gall bladder but is still produced in the liver and used for
digestion. Again, very few people with asymptomatic gall stones have any
need for treatment or surgery.
Surgical Treatment
Two main surgical techniques are used. One is the traditional
cholecystectomy where the abdomen is opened and the gall bladder and its
duct are tied off and removed. This requires general anesthesia and leaves
a significant scar under the right rib cage. President Lyndon Baines
Johnson demonstrates his gall bladder scar in a famous photograph of the
1960's. The recovery period for this is several weeks.
The alternative technique is much more popular today. It is called the
laparoscopic cholecystectomy. This technique uses three or four probes
inserted through tiny incisions in the abdominal wall to inflate the
abdomen with carbon dioxide, view the gallbladder lying behind and
underneath the liver, and remove the gallbladder and stones. The recovery
period is usually only a few days and scarring is nearly invisible.
Pilots/controllers undergoing these procedures may return to aviation
duties when cleared by their surgeon for full activity and they are
comfortable that they can perform all safety sensitive duties. Controllers
must also obtain clearance from the Regional Flight Surgeon before
returning to controlling. The operative report and discharge summary with
the surgeonís final note clearing the pilot/controller to return to
activity should be attached on the FAA Form 8500-8 at the next physical.
Follow up reporting is rarely required by the FAA.
Medical Treatment
Medical therapies to manage gallbladder disease are much less common than
surgical treatment. Only 10% of patients requiring treatment for
symptomatic gallbladder disease are candidates for medical treatment. One
technique uses medications alone to attempt to dissolve the stones. These
medications are called UDCA (ursodiol) and CDCA (chenodiol). They work
very slowly by decreasing cholesterol production in the liver. The
cholesterol in the stones is gradually diffused into the bile acid and
excreted in the intestine. About 50-60% of stones will dissolve over two
years. Use of these medications will require FAA review and approval
before flying or controlling. Remember, the underlying condition of
symptomatic gallstones may still be disqualifying, even if the medication
is tolerated well.
A newer medical therapy uses extracorporal shock waves, similar to the
technique used on kidney stones. The shock waves are focused on the stones
and attempt to blast them apart. Stones reform in about 20% of patients
and they generally are maintained on UDCA after treatment. Because of cost
and chances for recurrence, this treatment is not used often.
FAA Policy for Pilots & Controllers with Gallstones
The FAA will allow a pilot and controllers to perform duty with gallstones
that are not causing any symptoms. Frequently these stones are discovered
incidentally during another study such as an ultrasound or x-ray. If the
gallbladder is inflamed, a pilot or controller should not perform safety
sensitive duty during this period. In many cases, symptoms will resolve in
one to two weeks. They may then return to aviation duties and report the
episode at the next physical, if it resolves. Controllers should clear
through the Regional Flight Surgeons office before returning to work,
however. Those with chronic inflammation of the gallbladder are at risk
for recurrent attacks that may jeopardize flying safety. These individuals
should not fly or control until the problem is definitively corrected.
Pilots may return to flying after surgery for gallstones once the healing
is complete and their surgeon has released them to return to full
activity. Again, this surgery should be reported on FAA Form 8500-8 at the
time of the next physical examination. Reporting is not required for
pilots prior to the next examination if medications are not required. The
use of UDCA or CDCA for chronic treatment should be reported to the FAA
prior to returning to fly.
For controllers, reporting on the medical application is also required.
They must also clear through the Regional Flight Surgeon before retuning
to controlling duty. Remember, flying/controlling with active symptoms is
not appropriate.
|
